🤝 Elevating Concussion Care: The Power of Athletic Trainer and Physical Therapist Collaboration

Missouri Athletic Training Association Annual Meeting
What an amazing opportunity this past week to co-present with Dr. Carolina Quintana, ATC, PhD on how to capitalize on the Athletic Training/ Physical Therapist Relationship in Concussion Management!
We were able to ask hard questions on what common barriers and facilitators to collaborative practice and to summarize:
Barriers:
- Communication
- Lack of understanding of roles and responsibilities
- Lack of trust
Facilitators:
- Working for same organization
- Proximity to access to each other
- Understanding each other's scope of practice
Why Is This Important?
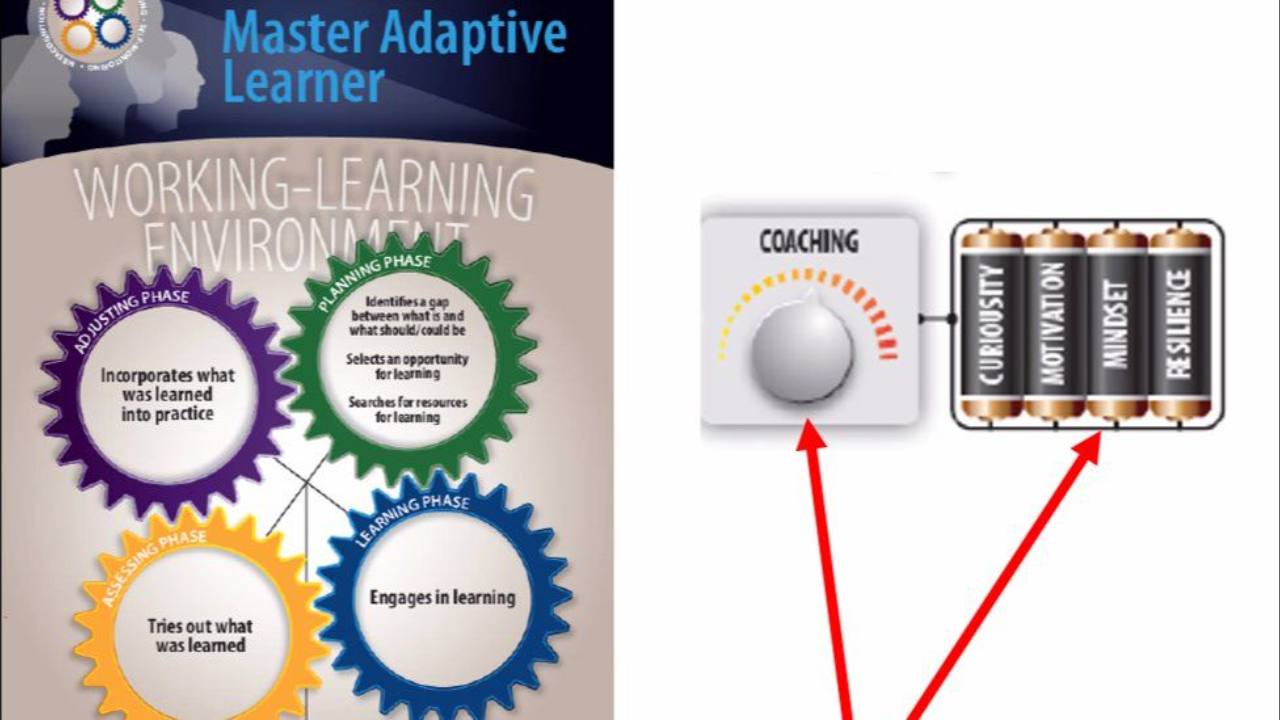
Concussion management in sport is a complex process that demands a truly interprofessional approach. Athletic Trainers (ATs) and Physical Therapists (PTs) play essential and complementary roles throughout the continuum of care—from acute injury recognition and sideline evaluation to long-term rehabilitation and return-to-play decisions.
Role of Athletic Trainers
ATs are often the first healthcare providers to assess a concussed athlete, providing immediate evaluation, stabilization, and symptom tracking. Their close proximity to athletes during practices and games allows them to initiate timely care and coordinate with the broader sports medicine team.
📌They also know these althletes inside and out (injury history, personality, coping strategies, parental structures, etc) This is SO important!
❓What about when Social Determinants of Health play a factor in care?
While research is still limited, early evidence suggests that certain social factors—like income, education, and support systems—may influence how well someone recovers from a concussion. When resources are limited ATs are posed to be able to provide access to care that may otherwise not be possible!
Physical Therapist Role
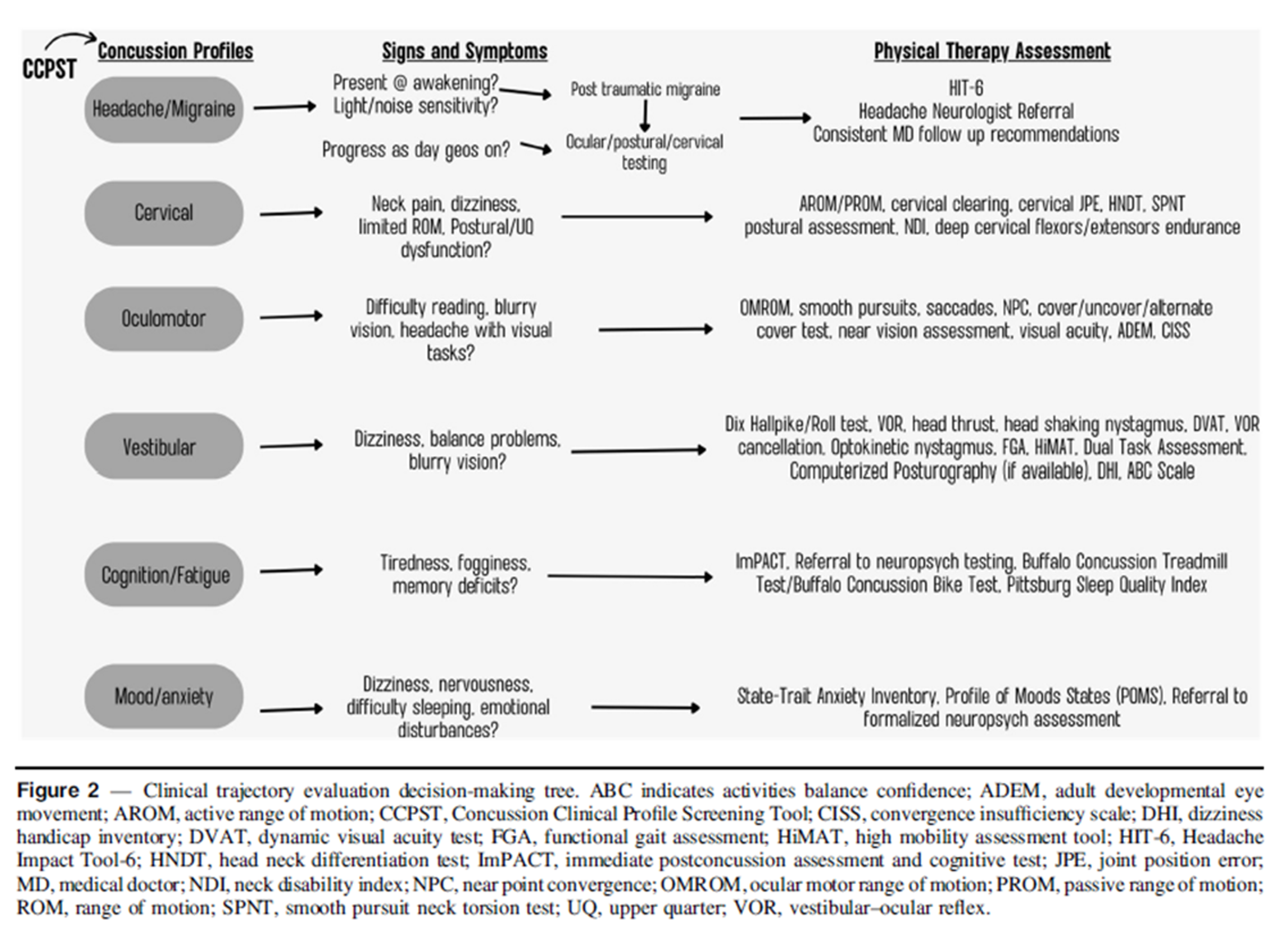
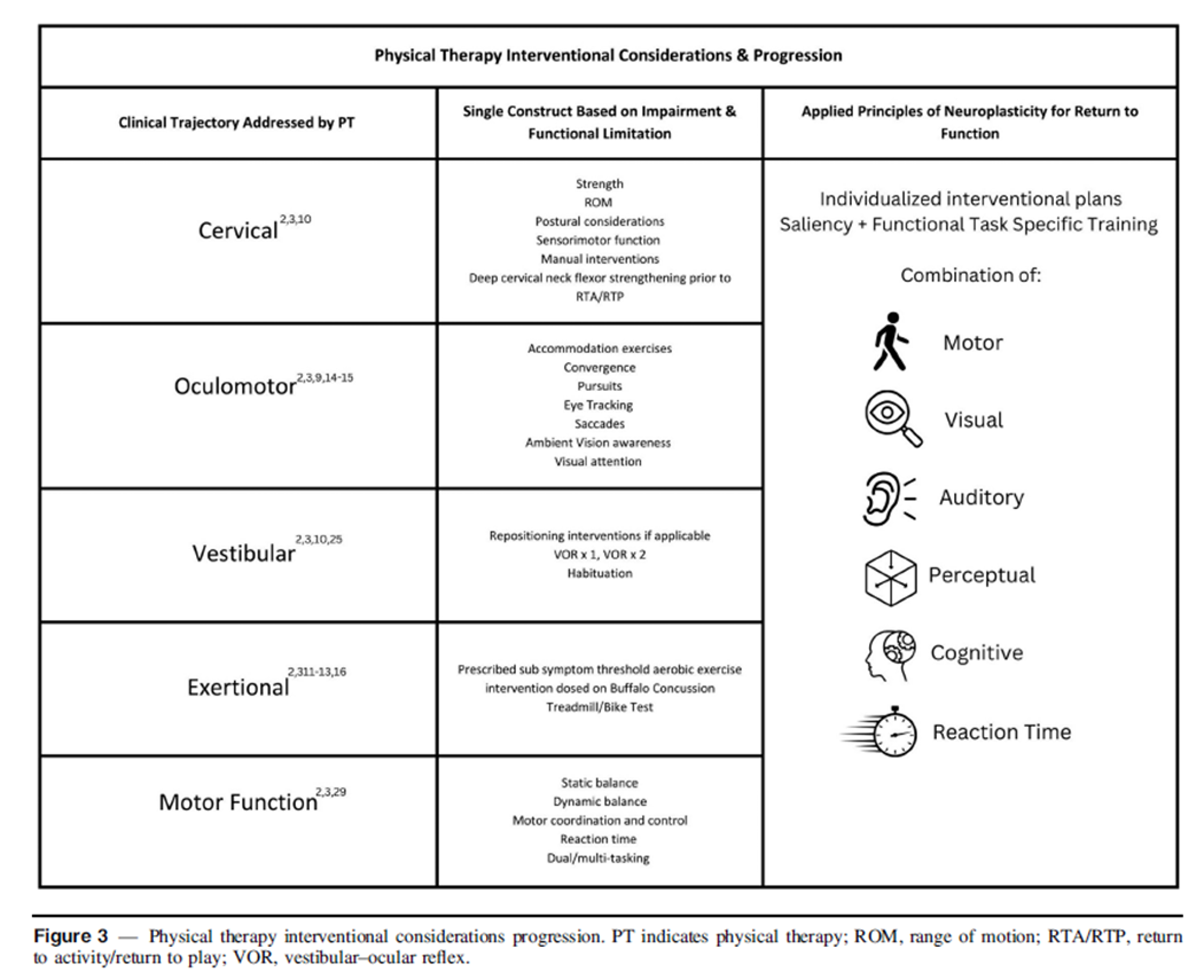
❗PTs bring specialized expertise in vestibular, oculomotor, and cervical spine dysfunctions—common aftereffects of concussion. Through targeted rehabilitation strategies, PTs help reduce symptoms like dizziness, imbalance, and neck pain, accelerating recovery and reducing the risk of prolonged symptoms.
PTs provide a comprehensive evaluation and targeted interventions to address clinical trajectories that patient's often experience following injury:
They also may have more time to dedicate to 1:1 rehab- think about a high school AT who has to cover 500+ athletes and has narrow windows to provide 1:1 care/rehab!
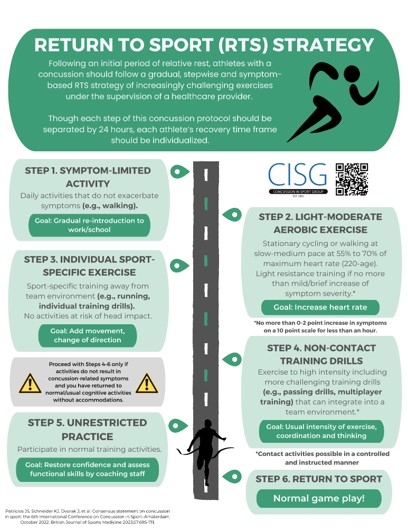
So working together this can be capitalized on with earlier return to safe practice activites that challenge the athlete based on principles of neuroplasticity:
Capitalizing on Collaboration
What makes this partnership powerful is shared communication, mutual respect for each profession’s scope of practice, and a coordinated management plan that centers on athlete safety.
✅This team-based model not only improves patient outcomes but also prevents complications such as second-impact syndrome and chronic post-concussive symptoms.
As concussion care continues to evolve, fostering strong AT-PT collaboration is essential for providing athlete-centered, evidence-informed care.
Helpful Strategies:
- Communicate early and often- as soon I see an athlete who has access to an AT I call them and give them a summary of findings as well as learn about the athlete's history of injury and personality!
- Shared rehab roles: often as a PT I only see the patient 1x a week with an extensive HEP- so I will let the AT know what they are doing with me and then this is carried over to practice (non-contact and safely) or in the Athletic Training room
- As a PT I take the athlete through stage 4 of the Return to Sport Protocol! This allows the AT to then easily progress to stage 5 when they are discharged from PT!
Open Honest Conversations Are 🔑
Would love to hear about how YOU foster this relationship!! Drop me a message! [email protected]
References:
- Hunt TN, Roberts K, Taylor EM, Quintana CP, Kossman MK. The Effect of Social Determinants of Health on Clinical Recovery Following Concussion: A Systematic Review. J Sport Rehabil. 2024 Mar 20;34(1):28-36. doi: 10.1123/jsr.2023-0068. PMID: 38508176.
- Patricios JS, Schneider KJ, Dvorak J, Ahmed OH, Blauwet C, Cantu RC, Davis GA, Echemendia RJ, Makdissi M, McNamee M, Broglio S, Emery CA, Feddermann-Demont N, Fuller GW, Giza CC, Guskiewicz KM, Hainline B, Iverson GL, Kutcher JS, Leddy JJ, Maddocks D, Manley G, McCrea M, Purcell LK, Putukian M, Sato H, Tuominen MP, Turner M, Yeates KO, Herring SA, Meeuwisse W. Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport-Amsterdam, October 2022. Br J Sports Med. 2023 Jun;57(11):695-711. doi: 10.1136/bjsports-2023-106898. PMID: 37316210.
- Bliss RA, Holland L, Fields C, Stock K. Use of Knowledge Translation Action Framework to Improve Physical Therapy Rehabilitation Outcomes in Concussion Management. J Sport Rehabil. 2024 Sep 25;34(3):335-345. doi: 10.1123/jsr.2024-0078. PMID: 39322212.


Responses